Decades of rigorous research has resulted in an overwhelming scientific consensus about Lyme disease diagnosis and treatment.
The scientific consensus has been affirmed by scientific reviews in the British Medical Journal and the Journal of the American Medical Association, and by medical and scientific groups around the world.
In line with the scientific consensus, in 2020, the Infectious Diseases Society of America, American Academy of Neurology, American College of Rheumatology, representatives from 12 other medical specialties, and patient representatives released comprehensive evidence-based guidelines.
An independent review published in the Journal of the American Medical Association rated the 2020 consensus guidelines as “good” or “good/fair” in all evaluated categories.
Additionally, an independent scientific panel conducted an exhaustive review of the science in 2010. The panel held an all-day public hearing and considered 1,025 references. An independent ombudsman certified each panel member as being free from conflicts of interest.
The independent panel unanimously upheld each of the recommendations made by the Infectious Diseases Society of America (IDSA) in 2006. Among other things, the panel concluded:
- In the case of Lyme disease, inherent risks of long-term antibiotic therapy were not justified by clinical benefit.
- To date, there is no convincing biologic evidence for the existence of symptomatic chronic B. burgdorferi infection among patients after receipt of recommended treatment regimens for Lyme disease.
The American Academy of Pediatrics said it more simply:
“Chronic Lyme disease” is not a medical diagnosis.
As of 2022, six randomized controlled trials and a number of other scientific studies provide strong evidence that Lyme disease patients do not benefit from long term antibiotics.
Those with “chronic Lyme” rarely had real Lyme
The pseudoscientific diagnosis called “chronic Lyme” should not be confused with symptoms stemming from authentic Lyme disease, including Lyme arthritis and post-Lyme symptoms.
The vast majority of people diagnosed with chronic Lyme disease never had Lyme infection in the first place. Therefore, any treatment for presumed Lyme disease would be inappropriate.
According to experts:
There are few better examples of health care fraud than the promotion of so called “chronic Lyme disease.”
Chronic Lyme stories typically exhibit many red flags, such as:
- diagnosis via pseudoscience practitioner (e.g. “Lyme literate”, functional, integrative, or naturopathic),
- clinical history and non-specific symptoms inconsistent with Lyme disease,
- a belief that an infection occurred years earlier,
- diagnosis in an area where real Lyme is rare or non-existent,
- multiple fake diagnoses, like alternate-universe versions of Bartonella and Babesia that bear no resemblance to the real infections,
- testing that is not positive or that uses unproven methodology,
- use of herbs/supplements
- outrageous treatment regimens, and
- others listed on our red flags page.
Scientists from the UK emphasize:
The epidemiology of so-called ‘chronic Lyme’ is more characteristic of a cultural phenomenon than an infectious disease. Public interest in Lyme disease has increased considerably due to ‘celebrity’ cases and discussion on social media.
A disturbing epidemic of false Lyme diagnoses
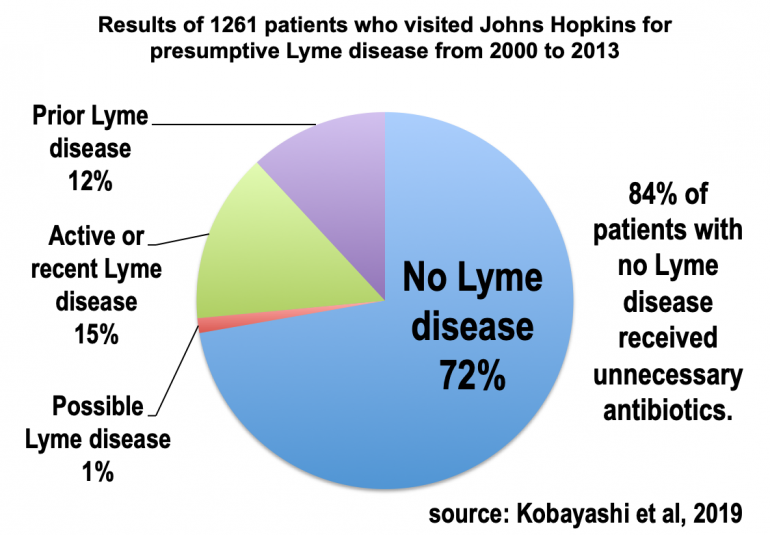
False positive Lyme disease diagnoses are very common, as found in a number of studies, including an exhaustive review of 14 years of visits to an infectious diseases clinic of the Johns Hopkins University School of Medicine.
In the Hopkins sample of 1261 patients, at least 72% of patients who visited for concerns about Lyme disease did not have the infection. Nevertheless, 84% of the patients with no Lyme disease received needless antibiotics. A follow-up study on the same sample noted that some patients had complications from the antibiotics, including C. difficile infection and venous thrombosis due to IV administration.
In the Hopkins study, roughly 2/3 of the 1061 patients without active Lyme disease were able to receive other diagnoses. The study found:
Leading diagnoses were anxiety/depression 222 (21%), fibromyalgia 120 (11%), chronic fatigue syndrome 77 (7%), migraine disorder 74 (7%), osteoarthritis 62 (6%), and sleep disorder/apnea 48 (5%).
Examples of less frequent but non-syndromic diseases newly diagnosed included multiple sclerosis (n = 11), malignancy (n = 8), Parkinson’s disease (n = 8), sarcoidosis (n = 4), or amyotrophic lateral sclerosis (n = 4).
ILADS Guidelines: “Potential harms”, “Not evidence-based”
Sadly, a dangerous anti-science group called ILADS has formed whose adherents have promoted all manner of quackery. Long term antibiotics are just one of numerous pseudoscientific and potentially dangerous modalities peddled by grifters associated with ILADS.
Experts have raised alarm about unethical practitioners claiming to be “Lyme literate”, including current or former ILADS leaders.
See more:
- Lancet Infectious Diseases: Antiscience and ethical concerns associated with advocacy of Lyme disease
- New England Journal of Medicine: A Critical Appraisal of “Chronic Lyme Disease”
- CDC: Serious Bacterial Infections Acquired During Treatment of Patients Given a Diagnosis of Chronic Lyme Disease
For example, ILADS leader Daniel Cameron, MD was disciplined after “allegations included practicing the profession of medicine with negligence on more than one occasion, incompetence on more than one occasion, gross negligence, gross incompetence, and/or failing to maintain accurate patient medical records.” Disturbingly, he was able to keep his medical license.
In addition to quack diagnoses of tick-borne diseases, ILADS leaders have promoted other unrecognized conditions, such as electromagnetic hypersensitivity, “toxic mold illness”/CIRS, and Morgellons.
Tellingly, ILADS admits all twelve of its 2014 recommendations—co-authored by Cameron—are based on “very low-quality evidence”. Infectious disease expert Mark Crislip, MD comments:
- What do you call a recommendation based on very low quality data? Belief. Belief is what you do in the absence of data.
- But more than basing their suggestions on low quality data, they ignore the fact that there is data that contradicts their position.
The above-mentioned British Medical Journal review states that the 2014 ILADS recommendations “have not provided any credible clinical or scientific evidence to support prolonged antibiotic therapy. Their designation as ‘evidence based guidelines’ belies their anecdotal nature and lack of coherent and evidence based guidance.”
In 2010, the Healthcare Protection Agency of UK—after noting the vulnerability of patients “desperate for an explanation and possible cure for their illnesses”—issued scathing conclusions about guidelines issued by ILADS:
- The ILADS guidelines are not evidence-based and are poorly constructed.
- Application of the ILADS guidelines’ poorly defined case definitions will result in a very high risk of misdiagnosis.
- Use of ILADS guidelines’ vague treatment recommendations, including prolonged use of antibiotics, has potentially serious consequences.
- Patients misdiagnosed with Lyme disease risk losing opportunities for diagnosis and treatment of other conditions. They also risk serious physical, psychological social and financial adverse events.
🌍 Experts agree around the world 🌎
Below are medical and science groups that support the scientific consensus about diagnosing and treating Lyme disease:
- 🇺🇸 Centers for Disease Control and Prevention (CDC)
- 🇺🇸 National Institutes of Health (NIH)
- 🇺🇸 Infectious Diseases Society of America
- 🇺🇸 American Academy of Family Physicians
- 🇺🇸 Pediatric Infectious Diseases Society
- 🇺🇸 American Academy of Neurology
- 🇺🇸 American College of Rheumatology
- 🇺🇸 American Academy of Pediatrics (2014 detailed guidelines)
- 🇺🇸 American Academy of Family Physicians
- 🇺🇸 American Academy of Dermatology (Review part 1 and part 2)
- 🇺🇸 National Association of Pediatric Nurse Practitioners
- 🇺🇸 Wilderness Medical Society
- 🇺🇸 Entomological Society of America
- 🇺🇸 American Lyme Disease Foundation (ALDF)
- 🇺🇸 Lyme MCW
- 🇺🇸 Science-based Medicine
- 🇺🇸 Mayo Clinic
- 🇺🇸 Cleveland Clinic
- 🇺🇸 American Medical Association
- 🌍 Child Neurology Society
- 🌍 European Academy of Neurology (supersedes the European Federation of Neurological Societies)
- 🌍 European Centre for Disease Prevention and Control
- 🌍 European Society of Clinical Microbiology and Infectious Diseases (ESCMID)
- 🌍 NorthTick (supported by the European Union, review)
- 🇬🇧 British Infection Association
- 🇬🇧 UK Health Security Agency (blog post)
- 🇬🇧 National Institute for Health and Care Excellence (NICE)
- 🇬🇧 British Society for Immunology
- 🇦🇺 Statement of Australian Scientists
- 🇦🇺 Australian Government Department of Health
- 🇦🇺 Australasian College of Dermatologists
- 🇦🇺 Australian Medical Association
- 🇦🇺 🇳🇿 The Royal Australasian College of Physicians
- 🇦🇺 Friends of Science in Medicine
- 🌏 Royal College of Pathologists Australasia
- 🇨🇦 Association of Medical Microbiology and Infectious Disease Canada
- 🇨🇦 Canadian Association for Clinical Microbiology and Infectious Diseases
- 🇨🇦 Canadian Medical Association
- 🇨🇦 Canadian Neurological Society
- 🇨🇦 Association des Medecins Microbiologistes Infectiologues du Quebec
- 🇨🇦 Public Health Physicians of Canada
- 🇨🇦 Canadian Paediatric Society
- 🇨🇦 College of Family Physicians of Canada
- 🇨🇦 National Collaborating Centre for Infectious Diseases (Canada)
- 🇨🇦 Public Health Agency of Canada
- 🇨🇦 Fédération des médecins spécialistes du Québec
- 🇨🇦 The Society of Obstetricians and Gynaecologists of Canada (La Société des obstétriciens et gynécologues du Canada)
- 🇨🇦 Nova Scotia Infectious Diseases Expert Group
- 🇮🇪 The Scientific Advisory Committee of the Health Protection Surveillance Centre (Ireland)
- 🇮🇪 The Infectious Diseases Society of Ireland
- 🇮🇪 The Irish Society of Clinical Microbiologists
- 🇮🇪 The Irish Institute of Clinical Neuroscience
- 🇮🇪 The Irish College of General Practitioners
- 🇧🇪 Belgian Federal Public Service Health, Food Chain Safety and Environment
- 🇧🇪 Belgian Antibiotic Policy Coordination Committee (BAPCOC)
- 🇧🇪 Belgian Society for Infectiology and Clinical Microbiology (Belgische Vereniging voor Infectiologie en Klinische Microbiologie/la Société Belge d’Infectiologie et de Microbiologie Clinique, BVIKM/SBIMC)
- 🇧🇪 Rheuma.be/Belgian Royal Society for Rheumatology (la Société Royale Belge de Rhumatologie, SRBR)
- 🇧🇪 Flemish Society for Neurology (la Société Flamande de Neurologie, VVN)
- 🇧🇪 Belgian Society of Internal Medicine (la Société Belge de Médicine Interne, SBMI)
- 🇧🇪 SSMG (la Société Scientifique de Médecine Générale, Belgian Scientific Society of General Medicine)
- 🇧🇪 Domus Medica
- 🇧🇪 Study Circle for Critical Evaluation of Pseudoscience and the Paranormal (SKEPP)
- 🇨🇿 Society for Infectious Diseases of the Czech Medical Association of J. E. Purkyně (English abstract)
- 🇨🇿 Czech State Health Institute (Statni Zdravotni Ustav, SZU)
- 🇩🇪 The Alliance for Child and Adolescent Health (Bündnis KJG))
- 🇩🇪 German Neurological Society (Deutsche Gesellschaft für Neurologie, DGN, additional warning to the public)
- 🇩🇪 German Dermatology Society (Deutsche Dermatologische Gesellschaft, DDG)
- 🇩🇪 German College of General Practitioners and Family Physicians (Deutschen Gesellschaft für Allgemeinmedizin und Familienmedizin, DEGAM)
- 🇩🇪 German Society for Occupational and Environmental Medicine (DGAUM)
- 🇩🇪 German Society of Oto-Rhino-Laryngology, Head and Neck Surgery (DGHNOKHC)
- 🇩🇪 German Society for Hygiene and Microbiology (Deutsche Gesellschaft für Hygiene und Mikrobiologie, DGHM)
- 🇩🇪 German Society for Immunology (DGfI)
- 🇩🇪 German Society of Infectious Diseases (DGI)
- 🇩🇪 German Society for Child and Adolescent Medicine (Deutsche Gesellschaft für Kinder und Jugendmedizin, DGKJ)
- 🇩🇪 German Society for Clinical Chemistry and Laboratory Medicine (Deutsche Gesellschaft für klinische Chemie und Laboratoriumsmedizin, DGKL)
- Society for Promoting Quality Assurance in Medical Laboratories (INSTAND)
- 🇩🇪 German Society for Pediatric Infectious Disease (Deutschen Gesellschaft für Pädiatrische Infektiologie, DGPI)
- 🇩🇪 The German Association of Psychiatry, Psychotherapy and Psychosomatics (Deutsche Gesellschaft für Psychiatrie und Psychotherapie, Psychosomatik und Nervenheilkunde, DGPPN)
- 🇩🇪 German Society of Psychosomatic Medicine and Medical Psychotherapy (DGPM)
- 🇩🇪 German College of Psychosomatic Medicine (DKPM)
- 🇩🇪 German Society for Rheumatology (Deutsche Gesellschaft für Rheumatologie, DGRh)
- 🇩🇪 German Pain Society (DGSS)
- 🇩🇪 German Ophthalmological Society (DOG)
- 🇩🇪 Paul Ehrlich Society for Chemotherapy (PEG)
- 🇩🇪 Robert Koch Institute
- 🇦🇹 Austrian Society of Dermatology and Venerology (ÖGDV)
- 🇦🇹 Austrian Society for Neurology (Österreichische Gesellschaft für Neurologie, ÖGN)
- 🇫🇷 National Academy of Medicine France (Académie nationale de médecine, see also 2016-09-20 statement)
- 🇫🇷 French High Council for Public Health (Le Haut Conseil de la santé publique)
- 🇫🇷 Health France (Santé publique France)
- 🇫🇷 The French Infectious Diseases Society (Société de Pathologie Infectieuse de Langue Française, SPILF)
- 🇫🇷 The French Association for Scientific Information (Association française pour l’information scientifique)
- 🇫🇷 French Society of Dermatology (Société française de dermatologie, SFD)
- 🇫🇷 French Society of Rheumatology (Société française de rhumatologie, SFR)
- 🇫🇷 French Federation of Neurology (Fédération française de neurologie, FFN)
- 🇫🇷 French Society of Neurology (Société française de neurologie, SFN)
- 🇫🇷 Collège national des généralistes enseignants (CNGE)
- 🇫🇷 College of General Practitioners (Collège de la médecine générale, CMG)
- 🇫🇷 Société nationale française de médecine interne (SNFMI)
- 🇫🇷 French Society of Microbiology (Société française de microbiologie, SFM)
- 🇫🇷 Collège National des professionnels en psychiatrie – collège national pour la qualité des soins en psychiatrie (CNPP-CNQSP)
- 🇫🇷 Association française de psychiatrie biologique et de neuropsychopharmacologie (AFPBN)
- 🇫🇷 Société de psychologie médicale et de psychiatrie de liaison de langue française (SPMPLLF)
- 🇫🇷 French Society of Occupational Medicine (Société française de médecine du travail, SFMT)
- 🇫🇷 French Society of Cardiology (Société française de cardiologie, SFC)
- 🇫🇷 French Society of Pediatrics (Société française de pédiatrie, SFP)
- 🇫🇷 Groupe de pathologies infectieuses pédiatriques (GPIP)
- 🇫🇷 Société française de rhumatologie et médecine interne pédiatrique (SOFREMIP)
- 🇫🇷 French Society of Ophthalmology (Société française d’ophtalmologie, SFO)
- 🇫🇷 French Society of Medical Mycology (Société française de mycologie médicale, SFMM)
- 🇫🇷 French Society of Parasitology (Société française de parasitologie, SFP)
- 🇫🇷 College of Professors of Infectious and Tropical Diseases (Collège des universitaires de maladies infectieuses et tropicales, CMIT)
- 🇫🇷 Collège national professionnel fédération française d’infectiologie (CNP-FFI)
- 🇫🇷 Centre National de Référence des Borrelia
- 🇫🇷 French National College of Gynecologists and Obstetricians (Collège National des Gynécologues et Obstétriciens Français, CNGOF)
- 🇫🇷 Société française d’étude et de traitement de la douleur (SFETD)
- 🇫🇷 French Association for Scientific Information (Association Française pour l’Information Scientifique)
- 🇭🇺 Hungarian Ministry of the Interior (and many experts listed as agreeing with the guideline)
- 🇪🇸 Spanish Society of Pediatric Rheumatology (Sociedad Española de Reumatología Pediátrica, SERPE)
- 🇪🇸 Spanish Society of Neurology (Sociedad Española de Neurología, SEN)
- 🇪🇸 Spanish Society of Immunology (Sociedad Española de Inmunología, SEI)
- 🇪🇸 Spanish Society of Pediatric Infectology (Sociedad Española de Infectología Pediátrica, SEIP)
- 🇪🇸 Spanish Society of Rheumatology (Sociedad Española de Reumatología, SER)
- 🇪🇸 Spanish Academy of Dermatology and Venereology (Academia Española de Dermatología y Venereología, AEDV)
- 🇪🇸 Spanish Association of Pediatrics (Asociación Española de Pediatría, AEP)
- 🇪🇸 Spanish Society of Infectious Diseases and Clinical Microbiology (Sociedad Española de Enfermedades Infecciosas y Microbiología Clínica, SEIMC)
- 🇳🇴 Norwegian National Advisory Unit on Tick-borne Diseases
- 🇳🇴 Norwegian Directorate of Health
- 🇳🇴 Norwegian Institute of Health
- 🇳🇴 Norwegian Children’s Association (Norsk barnelegeforening)
- 🇵🇱 Polish Supreme Medical Chamber (Naczelna Izba Lekarska, NIL)
- 🇵🇱 Polish Society of Epidemiology and Infectious Disease Physicians
- 🇵🇱 Polish Ministry of Health
- 🇨🇭 Swiss Society of Infectious Diseases
- 🇨🇭 Swiss Neurological Society
- 🇳🇱 Amsterdam Multidisciplinary Lyme Center (Amsterdam Multidisciplinair Lyme Centrum)
- 🇳🇱 Health Council of the Netherlands
- 🇳🇱 Dutch Foundation for Biosciences and Society
- 🇳🇱 Dutch Society for Dermatology and Venereology (Nederlandse Vereniging voor Dermatologie en Venereologie)
- 🇳🇱 Dutch Institute for Healthcare Improvement (CBO, with 17 other medical organizations listed below, pdf)
- 🇳🇱 Netherlands Association of Internal Medicine (Nederlandse Internisten Vereniging)
- 🇳🇱 Dutch College of General Practitioners (Nederlandse Vereniging van Revalidatieartsen)
- 🇳🇱 Netherlands Society of Emergency Physicians (Nederlandse Vereniging van Spoedeisende Hulp Artsen)
🇳🇱 Dutch Hospital Pharmacists Association (Nederlandse Vereniging van Ziekenhuisapothekers)
🇳🇱 Netherlands Society of Occupational Medicine (Nederlandse Vereniging voor Arbeids- en Bedrijfsgeneeskunde)
🇳🇱 Netherlands Society of Cardiology (Nederlandse Vereniging voor Cardiologie)
🇳🇱 Dutch Society for Dermatology and Venereology (Nederlandse Vereniging voor Dermatologie en Venereologie) - 🇳🇱 Dutch Association for Pediatrics (Nederlandse vereniging voor Kindergeneeskunde)
- 🇳🇱 Netherlands Society for Clinical Chemistry and Laboratory Medicine (Nederlandse Vereniging voor Klinische Chemie en Laboratoriumgeneeskunde)
🇳🇱 Dutch Society of Medical Microbiology (Nederlandse Vereniging voor Medische Microbiologie)
🇳🇱 Netherlands Society of Neurology (Nederlandse Vereniging voor Neurologie)
🇳🇱 Netherlands Psychiatric Association (Nederlandse Vereniging voor Psychiatrie)
🇳🇱 Dutch Society for Rheumatology (Nederlandse Vereniging voor Reumatologie)
🇳🇱 Dutch Association of Medical Insurance Physicians (Nederlandse Vereniging voor Verzekeringsgeneeskunde)
🇳🇱 Dutch Society for Infectious Diseases (Vereniging voor Infectieziekten) - 🇳🇱 National Institute for Public Health and the Environment (RIVM, Rijksinstituut voor Volksgezondheid en Milieu)
- 🇳🇱 Dutch College of General Practitioners (Nederlands Huisartsen Genootschap)
- 🇳🇱 Dutch National Care Institute (Zorginstituut Nederland)
- 🇩🇰 Danish Society of Infectious Diseases (Dansk Selskab for Infektionsmedicin)
- 🇩🇰 Danish Neurological Society (Dansk Neurolisk Selskab)
- 🇩🇰 Danish Society of Clinical Microbiology (Dansk Selskab for Klinisk Mikrobiologi)
- 🇸🇪 Swedish Medical Products Agency
- 🇸🇪 Swedish Council on Health Technology Assessment (English summary)
- 🇳🇴 🇸🇪 🇩🇰 🇫🇮 Nordic consensus on the assessment and follow-up of persons with long-term ailments after suspected tick-borne diseases (comment, English, norsk)
- 🇪🇪 Estonian Society for Infectious Diseases (Eesti Infektsioonhaiguste Selts, scientific review PDF)
- 🇲🇰 Ministry of Health for North Macedonia
- 🇫🇮 Guideline by Finnish doctors
- 🇦🇹 🇸🇮 Evidence review by scientists in Austria and Slovenia
- 🌎 Quackwatch
Other affirmations of support for science-based Lyme disease testing:
- 🇹🇷 Turkey Ministry of Health
- 🇺🇸 Association of Public Health Laboratories
- 🇺🇸 American Society for Microbiology
Studies show scientific consensus
Connecticut, USA study
A 2010 survey of Connecticut primary care physicians found 98% indicated they neither diagnosed nor treated presumed chronic Lyme disease.
British Study
In 2010, Dr. Sue O’Connell, a microbiologist who headed the Health Protection Agency Lyme Borreliosis Unit in the UK, performed a survey of Lyme diagnosis and treatment guidelines from 16 groups of medical experts in Europe and North America. She noted:
There is overall agreement regarding the clinical features of Lyme borreliosis and on the requirement for supporting laboratory evidence of a clinical diagnosis of later-stage infection. Two-tier serological testing, with immunoblot as a second-stage test, is currently recommended in most guidelines and reviews.
and:
No evidence-based European or North American guideline recommends prolonged or multiple courses of antibiotics for persistent symptoms following previously treated Lyme disease.
French Study
In 2018, a French review of European and American Lyme diagnostic guidelines noted “a global consensus.” This review concluded:
Contrary to the intense debate taking place on the Internet and in the European and American media, our analysis shows that the great majority of medical scientific guidelines with a high quality score, agree on the clinical diagnostic methods of Lyme disease.
Of the 16 guidelines reviewed in 2018 from 7 countries, only the guidelines of the pseudoscience group German Borreliosis Society (Deutsche Borreliose-Gesellschaft, DBG) were an outlier. DBG’s guidelines received the lowest quality score, 1. Similar to its America-based counterpart ILADS but unlike mainstream organizations, DBG recommended non-standard testing and defined a “chronic stage” of Lyme disease.
Presumably ILADS is not in the French review because no published diagnostic guidelines were available.
Independent Report from Washington State
In 2016, the Washington State Medical Quality Assurance Commission produced an independent report on the effects of long-term antibiotic treatment for Lyme disease.
The independent report acknowledged the overwhelming scientific consensus:
Long-term antibiotic treatment of “chronic Lyme disease” – a term the medical community doesn’t find meaningful – is not in patients’ best interest. Most patients with medically unexplained symptoms who received a diagnosis of post-treatment Lyme disease will require more than antibiotics to manage their symptoms. These patients should consult with their physician regarding a treatment plan that also includes emotional support, nutritional guidance and physical therapy. Practitioners should openly address any concerns and should reassure patients. Antibiotics are no substitute for sympathetic listening and explanation.
The benefits associated with long-term antibiotic treatments do not outweigh the risks to the residents of Washington. Evidence-based science has not determined the best long-term treatment option for post-treatment Lyme disease syndrome. Evidence-based treatments should remain the standard in Washington to ensure our residents’ safety.
In Washington State, Lyme disease cases are almost non-existent (generally only 0 to 3 endemic cases per year) and greatly outnumbered by fictional cases.
Other good sources
- U of Rhode Island TickEncounter Resource Center
- State and province public health departments
- Science-based doctors board certified in infectious disease, neurology, rheumatology, psychiatry, dermatology, pediatrics, and Allergy and Immunology
LymeScience resources
- Medical Child Abuse and “Chronic Lyme”
- Good journalism on “Chronic Lyme disease”
- Doctor and scientist commentaries on “Chronic Lyme”
- Papers on “Chronic Lyme disease”
- Papers describing a massive number of false positive Lyme diagnoses
- How “Chronic Lyme” recruits followers
- The harms of unnecessary “Lyme anxiety”
- Video: How fake medicine fools us
- From quack to science advocate: Personal journeys
Sources to avoid because they deny the scientific consensus
The harmful chronic Lyme movement started in the late 1980s and was described as a cult in a 2001 New York Times story. Allen Steere, one of the discoverers of Lyme disease, was being stalked and harassed by Lyme conspiracy theorists:
Early on, he tried to explain why, based on the science, he didn’t believe many of them had Lyme disease and, even if they did, why long-term antibiotics might not help. But none of it seemed to matter. On the Web, in virtual worlds Steere did not know or understand, patients who believed they had the paralyzing illness vilified him. Egged on by advocacy groups, they infected his sterile world, trying to destroy his reputation and career.
Much like Scientology, this movement was anti-psychiatry:
Because of the stigma of mental illness as well as the lack of cures for other diseases like fibromyalgia or chronic fatigue, they say, there is a constellation of forces pushing for such a diagnosis. Many companies often will not help mentally ill employees or those with poorly understood disorders like fibromyalgia; worse, insurance companies still don’t want to pay for long-term psychiatric care. As a result, they say, there is now a movement to treat other illnesses — including chronic fatigue syndrome and fibromyalgia — as Lyme disease and to attack doctors when they don’t.
Says one doctor in Steere’s camp: ”There is now a cult out there — these advocacy groups — that says to people: ‘This is not depression. This is not your fault. You have a spirochete in the brain. You should sue your doctor. What’s more, we’ll be your expert witness.”’
Steere puts it more philosophically. ”We’ve come to have the idea in America that it is possible to cure anything and that everyone could be well, and it’s even their right to be well, and they should be angry if the medical profession doesn’t make you well.”
A 1991 article in Harvard Health Letter reported on the “Lymeys” in a manner that still fits today:
Lymeys are unified by their belief that infection with the Lyme agent is the cause of their symptoms and by a general mistrust of standard medicine and its limitations. Many of them shun treatment at major medical centers known for research on Lyme disease. Instead, following what they read in the newsletters, some Lymeys travel great distances to consult self-appointed specialists with dubious credentials.
These doctors often prescribe intravenous antibiotic regimens lasting for months or, in extreme cases, years, at a cost of literally hundreds of thousands of dollars. Acting on physicians’ orders, private companies will administer intravenous drugs in patients’ homes. Some of these companies advertise their services in Lymey newsletters, help pay the publications’ costs, and publicize support groups.
Decades later, the bizarre beliefs of the “Lymeys” have been disproven over and over. Nevertheless, the chronic Lyme movement has supersized thanks to the internet, social media, celebrities, the wealthy, politicians, and quacks.
A 2004 study of web sites about Lyme disease revealed many that promoted inaccurate information. Web sites with information determined to be inaccurate tended to have the word “Lyme” in their names and included LymeDisease.org, IgeneX, ILADS, and Lyme Disease Association.
Sadly, the epidemic of misinformation about Lyme disease has only grown since 2004.
In 2017, March for Science had to cut ties with a pseudoscience group that falsely claimed to be representative of Lyme patients.
In 2018, scientists in the Department of Dermatology at Johns Hopkins University reported that sites such as Lymedisease.org are spreading inaccurate information about Bartonella, which is not a known tick-borne disease in North America or coinfection of Lyme disease.
Unfortunately, substantial confusion is caused by pseudoscience being legitimized in academia, almost entirely by initiatives funded by wealthy conspiracy theorists.
The easiest way to determine if an entity is dedicated to dangerous chronic Lyme pseudoscience is if it refers patients to predatory “Lyme literate” doctors or other practitioners of unscientific medicine (see below).
Follow the money
As of 2024, over $100 million has been pumped into promoting chronic Lyme pseudoscience, including funding universities and researchers who undermine long-settled science and who are inclined to violate basic standards of ethics. An example is ILADS leader Leona Gilbert, who was found guilty of scientific misconduct along with her business partner Kunal Garg.
In one of the more appalling scandals, US government employees dedicated taxpayer-funded resources to pump out anti-science and anti-patient propaganda and accepted millions of dollars from crank billionaires Steven and Alexandra Cohen. Additionally, Cohen-funded scientists appeared in the Cohen-produced conspiracy theorist documentary The Quiet Epidemic, which exploited an abused teenager.
We recommend avoiding the following:
- International Lyme and Associated Diseases Society (ILADS) [see the review from the UK’s Health Protection Agency]
- International Lyme and Associated Diseases Educational Foundation (ILADEF, the ILADS sister organization)
- LymeDisease.org and MyLymeData
- Global Lyme Alliance
- Bay Area Lyme Foundation (and associated entities Center for Lyme Action, Lyme Disease Biobank, and LaureL STEM foundation)
- Lyme Disease Association
- IgeneX
- NatCapLyme- The National Capital Lyme Disease Association and TickBusters.org
- Stand4Lyme
- Lyme Innovation
- PA Lyme Resource Network
- Lyme Action Network
- Colorado Tick-Borne Disease Awareness Association
- LivLyme Foundation
- Focus on Lyme
- Central New York Lyme and Tick-Borne Alliance
- Ride Out Lyme
- LymeNow
- Lyme Disease Awareness Foundation
- Partnership for Tick-borne Diseases Education, Lymecme.info, and other propaganda from ILADS leader Elizabeth Maloney
- Partner in Lyme
- Project Lyme and Generation Lyme
- The Avril Foundation
- Lyme Stats
- Mothers Against Lyme
- Band Aid Lyme
- Lyme Disease Foundation (Not to be confused with the science-based organization American Lyme Disease Foundation)
- The Mayday Project
- Midcoast Lyme Disease Support & Education
- Lyme Society, Inc.
- Florida Lyme Disease Association
- Lyme Connection
- LymeLight Foundation
- LymeHope
- Children’s Lyme Disease Network
- Twin Cities Lyme Foundation
- Minnesota Lyme Association
- Illinois Lyme Association
- Alex Hudson Lyme Foundation
- Chai for Lyme/Life for Lyme
- Infection and Autoimmunity Research and Education Foundation (IAREF)
- Lyme Treatment Foundation
- The Steven & Alexandra Cohen Foundation, TicksSuck.org, LymeX Innovation Accelerator, and any other projects associated with Steven and Alexandra Cohen
- MSIDS Research Foundation, The Lyme Initiative, and any other projects associated with Emily and Malcolm Fairbairn
- Autism Infectious Disease Association (AIDA)
- Southern Tier Lyme Support
- The Lyme Center
- MaineLyme
- LymeTV and Tick JEDI
- Lyme Education and Awareness Foundation (LEAF)
- Michigan Lyme Disease Association
- LymeDocs
- LymeBasics.org, formerly Lyme Disease Association of Southeastern Pennsylvania (LDASEPA)
- LymeLilli Foundation
- Lyme Association of Greater Kansas City, Inc
- Sam’s Spoons Foundation
- Lyme Disease Challenge
- Wisconsin Lyme Network
- Wayne County Lyme Disease Task Force
- The Mighty
- FlightPath Biosciences
- Open Medicine Institute & Howard Young Foundation’s Tick-Borne Illness Center of Excellence (Aspirus Tick-Borne Illness Center)
- Invisible International and the Montecalvo Platform for Tick-Borne Illness Medical Education, also marketed as VectorWise CME
- Tick Wise Education
- BioNeoMed Research Foundation
- Institute for Functional Medicine
- American Academy of Environmental Medicine
- American Board of Integrative Holistic Medicine
- American Academy of Anti-Aging Medicine (A4M)
- Association of American Physicians and Surgeons
- American College for Advancement in Medicine (ACAM)
- CanLyme – Canadian Lyme Disease Foundation
- Canadian Lyme Science Alliance (CLSA) and Canadian Lyme Consortium
- Association québécoise de la maladie de Lyme (AQML)
- Enfance Lyme Québec
- Caudwell LymeCo
- Lyme Disease UK
- Lyme Disease Action UK
- Lyme Resource Centre Scotland
- Academy of Nutritional Medicine (AONM)
- Tick Talk Ireland
- Karl McManus Foundation
- German Borreliosis Society (Deutsche Borreliose-Gesellschaft)
- Chronimed
- Fédération Française contre les Maladies Vectorielles à Tiques (FFMVT)
- France Lyme
- Le droit de guérir
- International Fund for Research on Lyme disease (I For Lyme)
- Lyme-Int
- Association Lyme Suisse
- Associazione Lyme Italia e coinfezioni
- NorVect – The Nordic Network for Vector-borne Diseases
- Global LymeXpert Group
- Lyme Disease Association of Australia [There is no compelling evidence you can contract real Lyme disease in Australia.]
- MSIDS Inc.
- PANDIS
- Australian Chronic Infectious and Inflammatory Disease Society (ACIIDS, formerly Australian Chronic Infectious Disease Society, ACIDS)
- Tick-borne Illness Community Network Australia Inc (TICNA)
- The International Society for Environmentally Acquired Illness (ISEAI)
- PolyBio Research Foundation
- Charles E. Holman Morgellons Disease Foundation
- Any other so-called Lyme patient group (other than this web site and the ALDF)
- Videos produced by chronic Lyme conspiracy theorists, such as Under Our Skin, The Quiet Epidemic, and “I’m Not Crazy, I’m Sick”
- Unscientific medicine practitioners, including those who market themselves using the following terminology: Lyme literate, integrative, functional, alternative, complementary, Traditional Chinese Medicine, holistic, natural, Biological, Ayurvedic, chiropractic, naprapathic, homeopathic, anti-aging, and naturopathic.
- Notoriously unreliable “wellness” web sites like Gwyneth Paltrow’s Goop, Verywell Health, Healthline (which includes Medical News Today and PsychCentral)
- Any organization listed by Quackwatch in their list of questionable organizations
- Projects, including in academia, that receive substantial funding and other support from chronic Lyme advocates, including:
- Brian Fallon and Shannon Delaney‘s Columbia University Lyme and Tick-Borne Diseases Research Center (“Columbia-Lyme.org”), the Cohen Center for Health and Recovery from Tick-Borne Diseases, and the unethical Lyme Clinical Trials Network (“LymeCTN”)
- David Putrino and Amy Proal’s Cohen Center for Recovery From Complex Chronic Illnesses (CoRE), and employees like Raven Baxter, who goes by “Raven the Science Maven” on Twitter/X
- LymeMIND and The Institute for Next Generation Healthcare at Icahn School of Medicine at Mount Sinai Health System
- Kristen Honey’s LymeX Innovation Accelerator at the U.S. Department of Health & Human Services (HHS)
- Initiatives at the National Academies of Sciences, Engineering, and Medicine (NASEM) unethically sponsored by the Steven & Alexandra Cohen Foundation, such as “Charting a Path Toward New Treatments for Lyme Infection-Associated Chronic Illnesses” and “Toward a Common Research Agenda in Infection-Associated Chronic Illnesses”
- The HHS Tick-Borne Disease Working Group, which:
- was dominated by anti-science and anti-patient activists (see Bloomberg coverage);
- heavily promoted predatory quacks, cranks, and perpetrators of Medical Child Abuse;
- produced reports riddled with dangerous lies and distortions;
- did not disclose in its reports the financial conflicts of interest of Working Group and subcommittee members; and
- failed to acknowledge the harms of chronic Lyme pseudoscience and the epidemic of false Lyme and “co-infection” diagnoses.
- Ying Zhang and Jie Feng’s group, formerly at Johns Hopkins University, later at Zhejiang University School of Medicine and Lanzhou University Medical College
- Nicole Baumgarth’s Johns Hopkins Lyme and Tickborne Diseases Institute
- John Aucott’s Johns Hopkins Lyme Disease Clinical Research Center and Lyme Disease Research Foundation (“HopkinsLyme.org”)
- Note: Researchers like John Aucott, Nicole Baumgarth, and Ying Zhang who promote dangerous pseudoscience groups and take money from them should not be confused with Hopkins professionals who are unconnected to pseudoscience groups.
- Kim Lewis’s group at Northeastern University
- Monica Embers‘s group at Tulane University
- Eva Sapi’s University of New Haven Lyme Disease Research Group
- The Dean Center for Tick Borne Illness (including associated individuals Charlotte Mao and Nevena Zubcevik)
- Vett Lloyd’s Mount Allison University/Maritime Lyme Research Network
- Melanie Wills’s G. Magnotta Lyme Disease Research Lab at University of Guelph
- Timothy Haystead’s group at Duke University, formerly associated with Neil Spector
- Mario Levesque and Matthew Klohn at Mount Allison University, and Marilyn Cox at Queen’s University
- Karl Morten’s group at University of Oxford
- Michal Caspi Tal’s group at MIT, formerly at Stanford
- Linda Griffith’s group at MIT
- Harvard’s Lyme Wellness Initiative
- Akiko Iwasaki’s group at Yale
- Brandon Jutras’s group at Northwestern, formerly Virginia Tech
- Those associated with the Bay Area Lyme Foundation’s unethical “Lyme Disease Biobank” such as Elizabeth Horn, Andrew Dwork, and Eric Gordon (who has history of misconduct).
- Natasha Rudenko, Maryna Golovchenko, and anyone else who denies the consensus that Lyme disease is not sexually transmitted.
- Publications by chronic Lyme advocates or authors funded by them, especially ones published in predatory or low-tier journals like Dove Medical Press, Frontiers, and MDPI.
Updated June 10, 2025