LymeScience republishes:
Internet-based self-diagnosis of Lyme disease caused death in a young woman with systemic lupus erythematosus
Zuzana Strizova a, Ondrej Patek b, Lenka Vitova b, Miroslava Horackova b, Jirina Bartunkova a
aDepartment of Immunology, 2nd Faculty of Medicine, Charles University in Prague and Motol University Hospital, V Uvalu 84, 15006, Prague 5, Czech Republic
bDepartment of Internal Medicine, 2nd Faculty of Medicine, Charles University in Prague and Motol University Hospital, V Uvalu 84, 15006, Prague 5, Czech Republic
Available online 17 January 2019, Version of Record 11 October 2019.
In the majority of cases; Lyme disease responds well to antibiotic treatment. Nevertheless; some patients may suffer from chronic nonspecific symptoms such as musculoskeletal pain and fatigue; termed as a post-treatment Lyme disease syndrome (PTLDS) [1]. The criteria for PTLDS diagnosis are clearly defined; however management of the condition by general practitioners is far from satisfactory [2]. Due to a symptomatology overlap, misinterpretation of PTLDS may lead to incorrect diagnosis of patients with autoimmune, neuromuscular or other somatic disorders, where identical symptoms are equally prevalent [3], [4]. Treatment recommendations for PTLDS are fiercely debated. Non-pharmacological approaches prevail while antibiotic treatment is strongly discouraged [4].
We report a 37-year-old female, a Faculty of Science graduate, with systemic lupus erythematosus (SLE) who was repeatedly misdiagnosed for a Lyme disease and treated with tetracycline antibiotics before she developed an acute exacerbation of SLE and finally died due to multi-organ failure.
The patient with a broad medical history (Fig. 1) experienced pericarditis, pleuritis and acute ischemic stroke at the age of 23 and was diagnosed with SLE. However, she refused to use immunosuppressive drugs and in agreement with opinions of several general practitioners concluded to have a diagnosis of chronic Lyme disease. The internet sources encouraged the patient to ask for repetitive serology testing and to demand further antibiotic treatment for Lyme disease. Despite a strong evidence supporting a causative role of tetracycline antibiotics in drug-induced lupus (DIL), the patient was repetitively treated for 10 years with either Minocycline or Doxycycline [5].
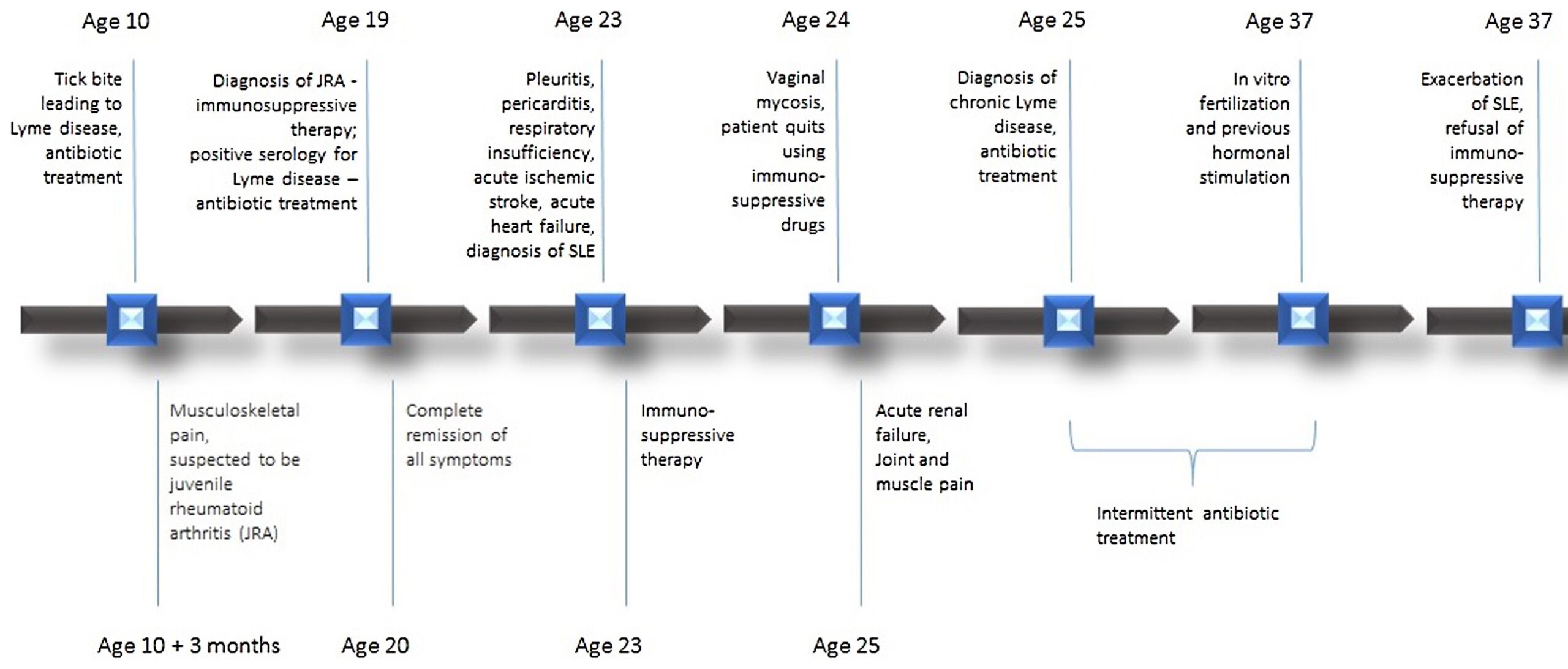
Fig. 1. Medical events in a 37-year-old female with untreated systemic lupus erythematosus in chronological order.
Before the admission, the patient underwent in vitro fertilization (IVF) after previous hormonal stimulation, which presumably exacerbated her condition [6].
During the hospitalization, the patient reached more than 10 criteria according to SLICC classification (Table 1) and with respect to the established diagnosis of SLE was advised to start immunosuppressive treatment. This approach, however, was rejected by the patient who did not accept the diagnosis and remained deeply convinced that Borrelia burgdorferi is the cause of her symptoms. Whether the neuropsychiatric SLE (NPSLE) could have affected the decision making of the patient could not be examined, although evidence of executive functioning deficits in SLE patients has already been reported [7].
Table 1. Results of immunological laboratory testing the day after the admission to Motol University Hospital. The results supported the diagnosis of SLE according to SLICC criteria.
| C3 | 0.33 | 0.83–2.25 |
|---|---|---|
| C4 | 0.04 | 0.14–0.35 |
| ANA pattern | homogenous | |
| ANA IgG | positive titer 1:2560 | |
| ANA IgA | positive titer 1:80 | |
| ANA IgM | positive titer 1:80 | |
| ds-DNA | positive titer 1:320 | |
| aCLA IgG | 7.1 GLP/mL | 0.00–11.0 |
| ENA screening IP | > 3.50 | 0.00–1.00 |
| Sm | 0.66 | 0.00–1.20 |
| RNP | 0.96 | 0.00–1.20 |
| SS-A | > 3.50 | 0.00–1.20 |
| SS-B | > 3.50 | 0.00–1.20 |
| RF IgG | 13.1 IU/mL | 0.0–22.00 |
| RF IgA | > 100.0 IU/mL | 0.0–22.00 |
| RF IgM | > 100.0 IU/mL | 0.0–22.00 |
| ACPAs | 1.50 U/mL | 0.00–4.00 |
Nonetheless, the patient kept continually refusing immunosuppressive therapy. The systemic autoimmunity progressed, and led to a multi-organ failure, regardless an intensive life support therapy.
We aim to highlight that knowledge of recent guidelines for diagnostics and treatment of Lyme disease is crucial. There is clear evidence that positive serology does not indicate infection with B. burgdorferi and most importantly, antibiotic therapy for PTLDS is potentially harmful [4], [8]. We report that the patient’s internet-based self-diagnosis of Lyme disease and repetitive misdiagnosis by physicians led eventually to the refusal of immunosuppressive treatment and the patient’s death. Furthermore, it is strongly advised to search for immune dysregulations before providing IVF as the whole procedure may cause thromboembolic complications and/or flare in the majority of autoimmune diseases [9], [10]. Also careful investigation of drugs associated with DIL seems to be of particular importance in patients with lupus-like clinical phenotypes.
Disclosure of interest
The authors declare that they have no competing interest.
The manuscript has been approved for publication by all authors and is not currently under review or submitted to another journal.
References
[1] Aucott JN, Rebman AW, Crowder LA, et al. Post-treatment Lyme disease syndrome symptomatology and the impact on life functioning: is there something here? Qual Life Res 2013;22:75–84. [2] Seriburi V, Ndukwe N, Chang Z, et al. High frequency of false positive IgM immunoblots for Borrelia burgdorferi in clinical practice. Clin Microbiol Infect 2012;18:1236–40. [3] Uhde M, Indart A, Fallon BA, et al. C-reactive protein response in patients with post-treatment Lyme disease symptoms versus those with myalgic encephalomyelitis/chronic fatigue syndrome. Clin Infect Dis 2018;67:1309–10. [4] Nemeth J, Bernasconi E, Heininger U, et al. Update of the Swiss guidelines on post-treatment Lyme disease syndrome. Swiss Med Wkly 2016;146:w14353. [5] Sturkenboom MC, Meier CR, Jick H, et al. Minocycline and lupuslike syndrome in acne patients. Arch Intern Med 1999;159:493–7. [6] Orquevaux P, Masseau A, Le Guern V, et al. In vitro fertilization in 37 women with systemic lupus erythematosus or antiphospholipid syndrome: a series of 97 procedures. J Rheumatol 2017;44:613–8. [7] Leslie B, Crowe SF. Cognitive functioning in systemic lupus erythematosus: a meta-analysis. Lupus. 2018. [8] Seriburi V, Ndukwe N, Chang Z, et al. High frequency of false positive IgM immunoblots for Borrelia burgdorferi in clinical practice. Clin Microbiol Infect 2012;18:1236–40. [9] Costa M, Colia D. Treating infertility in autoimmune patients. Rheumatology (Oxford) 2008;47:38–41 [10] Bellver J, Pellicer A. Ovarian stimulation for ovulation induction and in vitro fertilization in patients with systemic lupus erythematosus and antiphospholipid syndrome. Fertil Steril 2009;92:1803–10.Citation: Strizova Z, Patek O, Vitova L, Horackova M, Bartunkova J. Internet-based self-diagnosis of Lyme disease caused death in a young woman with systemic lupus erythematosus. Joint Bone Spine. 2019 Oct;86(5):650-651. doi: 10.1016/j.jbspin.2018.12.011. Epub 2019 Jan 17.
The final form of this article was published in Joint Bone Spine. This manuscript is republished in accordance with Elsevier’s sharing policy and is licensed under a Creative Commons license (CC-BY-NC-ND 4.0).
The above article has been adapted for internet display by the LymeScience Document Repository and posted with author permission.
Articles by the same team:
Strizova Z, Smrz D, Bartunkova J. Seroprevalence of Borrelia IgM and IgG Antibodies in Healthy Individuals: A Caution Against Serology Misinterpretations and Unnecessary Antibiotic Treatments. Vector Borne Zoonotic Dis. 2020.
Strizova Z, Smrz D, Bartunkova J. Response to Weiss MF re: “Seroprevalence of Borrelia IgM and IgG Antibodies in Healthy Individuals: A Caution Against Serology Misinterpretations and Unnecessary Antibiotic Treatments”. Vector Borne Zoonotic Dis. 2020.