Lyme disease is a curable infection according to global scientific consensus. It can be diagnosed via testing or symptoms such as a characteristic rash that occurs in the vast majority (70-90%) of patients.
Lyme bacteria (Borrelia burgdorferi) also takes 36-48 hours or more to transmit, which is a reason why in endemic areas, only about 2% of bites from discovered ticks result in infection.
The infection is also very geographically and seasonally restricted. Borrelia burgdorferi does not release harmful toxins, and deaths are extraordinarily rare.
However, the American Academy of Pediatrics warns:
Misinformation about chronic Lyme disease on the Internet and in popular media has led to publicity and anxiety about Lyme disease that is out of proportion to the actual morbidity that it causes.
False positive Lyme diagnoses
Scientists have witnessed for decades how people have been falsely diagnosed with Lyme disease, in particular those with medically unexplained symptoms, including Chronic Fatigue Syndrome and Fibromyalgia.
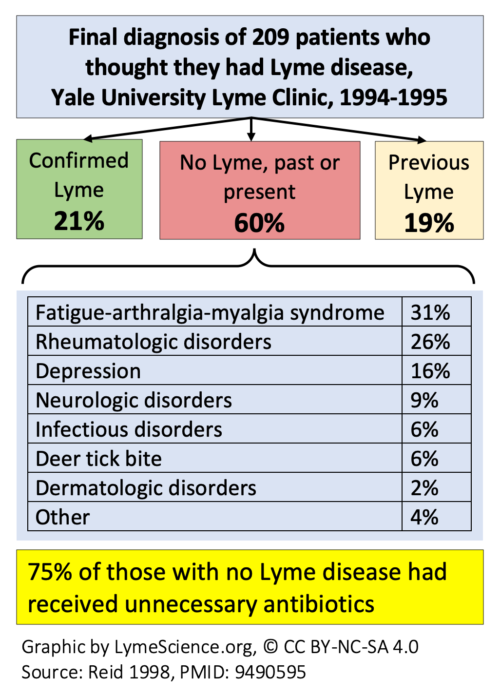
In a 1998 study from Yale of 209 patients with Lyme diagnoses, 60% never had Lyme disease. In that group, patients had a median of four Lyme tests, seven doctor’s visits, and 42 days of antibiotic treatment.
The patients had a number of diagnosable conditions listed below:
For a true Lyme infection, treatment is typically 10-28 days. Additionally, testing is neither necessary nor recommended if exposure history and symptoms like the distinctive rash clearly point to a diagnosis.
Testing is also not recommended without exposure history and appropriate physical exam findings, and a second test is generally only used if the first test was performed within weeks of infection.
But according to the CDC:
- Patients who have had Lyme disease for longer than 4-6 weeks, especially those with later stages of illness involving the brain or the joints, will almost always test positive.
- A patient who has been ill for months or years and has a negative test almost certainly does not have Lyme disease as the cause of their symptoms.
In the Yale study, 55% of the patients had at least one minor adverse drug event and 6% had a major adverse drug reaction like C. Diff. Depression and stress were very high in the group, at 42% and 45%, respectively.
Chronic Lyme: Real vs fake
As with other pseudosciences, chronic Lyme intermixes facts with fiction so it’s difficult to tell the difference.
Real Lyme infections can persist without treatment. Therefore, in Europe and in early scientific literature, both untreated Lyme disease and post-treatment symptoms have been referred to as “chronic.” As the CDC and NIH emphasize, experts stopped using the phrase “chronic Lyme” because of confusion over all the ways it was used.
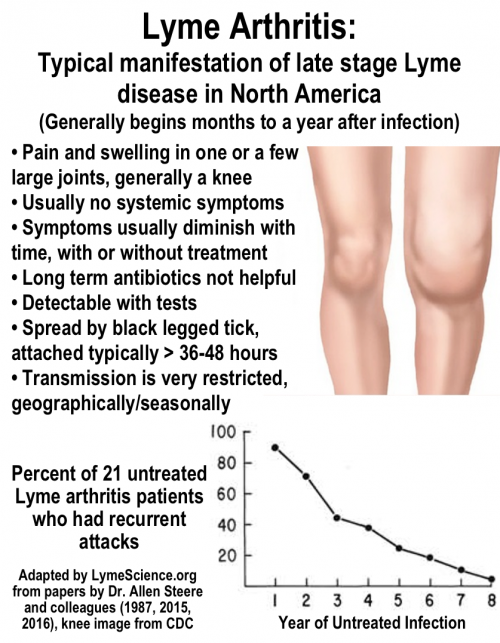
Most diagnoses of Lyme disease are referred to as “early” because they occur within weeks to months of infection. Late stage Lyme disease is rare, but confusion about it runs rampant. In North America, the typical manifestation of late stage Lyme is Lyme arthritis, described in the graphic below:
In Europe, there is also a skin manifestation of late stage Lyme disease called acrodermatitis chronica atrophicans.
Scientists like Dr. Allen Steere started studying the phenomenon of Lyme arthritis in the 1970s, before it was known to be caused by bacteria. In a 1987 paper, Steere and colleagues examined 55 patients who had untreated Lyme rashes.
Out of the 55 patients with an untreated Lyme rash, 11 (20%) had no other manifestations of Lyme disease while 44 (80%) developed types of joint pain. As shown in the graph above, a subset of patients who had recurrent attacks of Lyme arthritis tended to have their symptoms improve—and even disappear—over time.
It is important to differentiate Lyme arthritis from other causes of arthritis. Since Lyme arthritis is generally localized to the large joints, it’s also quite different from diffuse pain that might accompany other disorders, such as fibromyalgia.
Deceptive Lyme symptom questionnaires sow fear
Sometimes lengthy lists of non-specific symptoms are used to justify a false chronic Lyme diagnosis. Research has found that these lists are not helpful because such symptoms are common in the population. Dr. Harriet Hall reviewed one of these symptoms lists and wondered if it could be used to diagnose everyone with chronic Lyme disease.
The following is an excerpt from the 1998 book Lyme Disease about the phenomenon of “Lyme anxiety”. It’s still relevant today, especially given the role of social media in spreading even more unnecessary anxiety and false information.
The section is by Dr. Leonard Sigal, who has written extensively about Lyme disease misconceptions.
Lyme anxiety is common in and near areas endemic for Lyme disease. There is widespread concern that Lyme disease is incurable and that this infection can only be brought into temporary remission and will continue to flare.
With widespread anxiety about Lyme disease has come Munchausen syndrome and Munchausen syndrome-by-proxy in those concerned about “chronic” Lyme disease. The psychologic and financial costs of the misdiagnosis and treatment of “chronic” Lyme disease are staggering but have not been considered in most discussions of the public health burden of the mismanagement of Lyme disease.
In some of the patients with “Lyme anxiety,” no objective evidence of inflammation or infection is found, preceding or current, and serologic evidence of prior exposure to B. burgdorferi may or may not be present. Quite often, a low-positive ELISA result is the only such evidence, raising concerns of false-positive serologic testing. Not infrequently such patients have sought the advice of support groups or local “Lyme disease experts.”
This category of illness represents an enlarging majority of the “chronic Lyme disease” population. Such patients have often been tested repeatedly, often with tests of no value (e.g., urinary antigen tests), and have been subjected to many courses of antibiotics, often with agents of no proven efficacy. Many patients have found a place in their personas for “chronic Lyme disease,” and this may be the most permanently damaging aspect of Lyme disease.
In response to anxiety about Lyme disease has come a trend toward antibiotic regimens of greater duration or dose and combinations of antibiotics. However, this increased exposure to antibiotics results in a greater risk of adverse reactions to therapy. Not infrequently, drug side effects have been misinterpreted as manifestations of Lyme disease and occasionally labeled as “delayed Herxheimer reactions.”
Diarrhea in the setting of chronic antibiotic therapy has been called “Lyme colitis,” an entity that has never been described in the peer-reviewed medical literature, rather than Clostridium difficile enteropathy; several patients with this condition have responded well to vancomycin therapy, prompting some clinicians to claim that vancomycin is a cure for borrelial enteropathy.
With the emergence of enterococcus and perhaps Staphylococcus aureus resistant to vancomycin, the unnecessary use of this agent is to be avoided. Especially in patients receiving long-term antibiotic therapy, further antibiotic treatment is not warranted.
A detailed evaluation to ensure that no other illness is present is needed, with special attention to possible fibromyalgia. Such patients need reassurance and education, not medication, to feel comfortable with their new understanding that they do not have Lyme disease.
Dr. Paul Offit has observed, “While it’s very easy to scare people, it’s much harder to unscare them.”
Videos by Dr. Sigal
What Is “Lyme Anxiety?”
Treatment Approach for Patients with Potential Lyme Anxiety
Why Might Lyme Disease Be Overdiagnosed or Overtreated?
Consequences to Long-Term Antibiotic Therapy
Other videos
See full article: How Chronic Lyme recruits followers
Risk Bites: Why Aren’t We More Scared of Measles?
More discussion of risk at SciMoms.
Other resources
ScienceNews: Five reasons to not totally panic about ticks and Lyme disease
New York Times: My Son Got Lyme Disease. He’s Totally Fine
Caputo GM. Lyme anxiety. JAMA. 1991;266(3):359.
Shapiro ED, Gerber MA. Lyme Disease. Clinical Infectious Diseases 2000;31:533-542
LymeScience: Medical Child Abuse
Sigal LH. Misconceptions about Lyme disease: confusions hiding behind ill-chosen terminology. Ann Intern Med. 2002;136(5):413-9.
Sigal LH. Summary of the first 100 patients seen at a Lyme disease referral center. Am J Med. 1990;88(6):577-81.
Sigal LH. Anxiety and persistence of Lyme disease. Am J Med. 1995
Rorat M, et al. [Growing boreliosis anxiety and its reasons]. Psychiatr Pol. 2010;44(6):895-904.
Melia MT, et al. Lyme disease: authentic imitator or wishful imitation? JAMA Neurol. 2014;71(10):1209-10.
The Guardian: Health anxiety is not a joke – it can ruin lives
Bustle: Health Anxiety Is Way More Than Being A Hypochondriac — And It’s Way More Common Than You Think
Anxiety and Depression Association of America: Health Anxiety: What It is and How to Beat It
Anxiety and Depression Association of America: The facts about health anxiety
SciMoms: Risk in Perspective
Updated December 14, 2023