Table of contents
What is MARCoNS?
MARCoNS is a diagnosis not recognized by medical science that is an abbreviation of Multiple Antibiotic Resistant Coagulase Negative Staphylococci. Proponents of fake MARCoNS diagnoses claim it is a type of antibiotic resistant staph that can be found deep in the nose.
Those who diagnose MARCoNS are typically incompetent quacks. These quacks may advertise themselves using terminology such as “integrative”, “functional”, “Lyme literate”, or “holistic”. Many quacks are well-meaning and sincerely believe in what they’re selling.
MARCoNS is associated with those who believe in other unrecognized conditions such as “toxic mold illness”, sometimes called biotoxin illness or Chronic Inflammatory Response Syndrome (CIRS). CIRS was made up by Ritchie Shoemaker, a doctor who stopped practicing medicine after being disciplined by the Maryland Medical Board.
MARCoNS Symptoms
Since MARCoNS is not a real diagnosis, it would be a mistake to attribute symptoms to it. However, many quacks use misleading questionnaires to wrongly explain symptoms.
Dr. Jonathan Howard, a neurologist, details how these questionnaires exploit our psychology by using the Forer Effect, also called the Barnum Effect. This is when statements that apply to many different people seem quite specific.
Evidence for MARCoNS
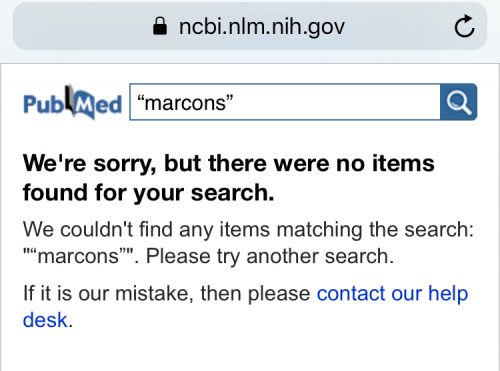
There is no compelling evidence to support MARCoNS diagnosis and treatment. A 2018 search of PubMed for papers about MARCoNS returned no results for the purported sinus infection.
A 2018 search of PubMed Commons (a different database) returned two papers, both authored by Dale Bredesen. Bredesen makes questionable claims about being able to treat Alzheimer’s disease. Bredesen provides no evidence that MARCoNS exists.
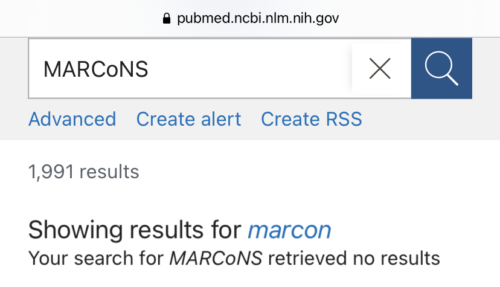
We received messages from advocates for MARCoNS disputing our PubMed search. These advocates overlooked that when PubMed finds no results, it changes the search term to one that does return results.
A 2021 PubMed search for MARCoNS also revealed no results while automatically listing 1,991 results for an unrelated term “marcon.”
Macarons are delicious treats and should also not be confused with the fake MARCoNS diagnosis.

MARCoNS treatments
No ethical doctor would prescribe a treatment for a diagnosis that isn’t real, like MARCoNS.
It’s important to understand that drug development is not easy. Safety, efficacy, dosage, and cost are all important factors. Thus, miracle claims made by practitioners of unproven and disproven treatments need to be questioned.
To learn more about pharmacology, please see our page about supplements and herbs.
BEG Spray
A nasal spray called BEG (containing Bactroban, EDTA, and gentamicin) is advertised as a treatment for MARCoNS. This is not a drug combination used in mainstream medicine. Its safety and efficacy are unknown.
No ethical doctor would prescribe BEG nasal spray because it has not been adequately tested in humans.
See also: Video: How fake medicine fools us
Beware predatory compounding pharmacies
BEG Spray is not an FDA approved drug. But compounding pharmacies are not regulated the same way as pharmaceutical companies. Hence, some unscrupulous compounding pharmacies are allowed to sell the bizarre BEG drug cocktail.
LymeScience recommends against patronizing the following pharmacies: Woodland Hills Pharmacy, The Compounding Lab Australia, Forte Rx, The Compounding Center, Infuserve America, and Hopkinton Drug Compounding and Wellness
Colloidal silver
Colloidal silver is also advertised for MARCoNS. According to the NIH:
- Scientific evidence doesn’t support the use of colloidal silver dietary supplements for any disease or condition.
- Colloidal silver can cause serious side effects. The most common is argyria, a bluish-gray discoloration of the skin, which is usually permanent.
- Colloidal silver can also cause poor absorption of some drugs, such as certain antibiotics and thyroxine (used to treat thyroid deficiency).
- The FDA also warned in 1999 that colloidal silver isn’t safe or effective for treating any disease or condition.
- The FDA and the Federal Trade Commission have taken action against a number of companies for making misleading claims about colloidal silver products.
Colloidal silver won’t help but can turn you blue
MARCoNS testing
Several questionable labs advertise testing for MARCoNS, including Microbiology DX of Bedford, MA and NutriPATH of Victoria, Australia. LymeScience does not recommend patronizing these labs.
Sounds Sciency
Many forms of pseudoscience use sciency-sounding words to appear legitimate. In the case of a fake MARCoNS diagnosis, it is based on a real group of bacteria called coagulase-negative staphylococci (CoNS or CNS).
In reality, CoNS are typically naturally found in healthy people. It is normal to find CoNS on our skin.
Even if a test were to accurately determine a patient carried a type of CoNS, the clinical significance of the finding would be highly questionable. The CoNS could be essentially an innocent bystander being blamed for completely unrelated symptoms.
Resources
Becker K, et al. Coagulase-negative staphylococci. Clin Microbiol Rev. 2014;27(4):870-926.
Helewa RM, Embil JM. What to do with Coagulase-Negative Staphylococci. The Canadian Journal of CME. 2007.
Updated March 16, 2021
Macarons image CC-BY-2.0 by Julien Haler