Despite false information online, Lyme disease is quite geographically restricted. The CDC reports “in 2015, 95% of confirmed Lyme disease cases were reported from 14 states.” This creates a natural experiment where it’s possible to see if Lyme incidence in areas of high Lyme disease incidence correlates to any other diseases.
Lyme disease has been blamed—with no compelling evidence—for autism, Alzheimer’s disease, Amyotrophic Lateral Sclerosis (ALS aka Motor Neuron Disease, MND, or Lou Gehrig’s Disease), Multiple Sclerosis (MS), Parkinson’s Disease, cancers, and suicides.
Chronic Lyme activists falsely state that Lyme disease either causes or commonly “mimics” just about everything. But is any of this true? These are testable hypotheses.
Additionally, experts note that Lyme disease and other neurological disorders are easy to differentiate:
Patients with Lyme disease do not exhibit the white matter plaques seen on imaging of patients with multiple sclerosis, for example, and when patients with Lyme disease have oligoclonal bands in their cerebrospinal fluid, they are actually reactive against B burgdorferi. Lyme disease does not produce the upper motor neuron signs seen in amyotrophic lateral sclerosis.
Table of contents
ALS, MS, Parkinson’s disease, and Alzheimer’s disease: No link to Lyme disease
In 2018 and 2019, scientists reviewed 30 years of Danish medical records of patients diagnosed with Lyme neuroborreliosis. They found no connection between neuroborreliosis and any of ALS, MS, Parkinson’s disease, and Alzheimer’s disease.
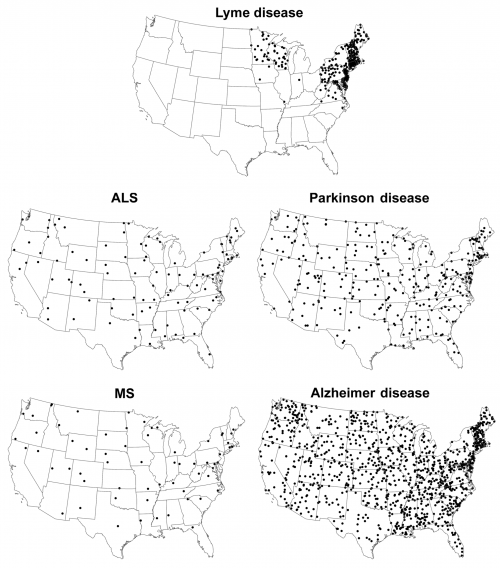
In 2015, CDC scientists compared Lyme disease prevalence to death rates for ALS, MS, Parkinson’s disease, and Alzheimer’s disease, as illustrated in the figure below. Like in Denmark, the CDC scientists found no link between Lyme disease and any of ALS, MS, or Parkinson’s.
Experts recommend against testing
In 2020, the expert panel that wrote the consensus Lyme disease guidelines noted the lack of associations between Lyme disease and ALS, MS, Alzheimer’s, or Parkinson’s. The panel strongly recommended:
In patients with typical amyotrophic lateral sclerosis, relapsing-remitting multiple sclerosis, Parkinson’s disease, dementia or cognitive decline, or new-onset seizures, we recommend against routine testing for Lyme disease (strong recommendation, low-quality evidence).
The rationale for the panel’s recommendation included the following:
These recommendations place a high value on avoiding false positive Lyme disease test results, which can delay appropriate medical evaluation and treatment of other disorders and lead to unnecessary antibiotic exposure and potential side effects. Screening neurologic patients with a low a priori likelihood of Lyme disease—that is, without a history of tick bite, erythema migrans, or other more typical manifestations, would result in far more false positive than true positive results.
Alzheimer’s
The CDC scientists mentioned above also found a small inverse correlation between Alzheimer’s disease deaths and Lyme disease. Where Lyme disease was high, Alzheimer’s disease death rates were lower. So does Lyme disease prevent Alzheimer’s? Probably not. But regardless, the CDC scientists were able to conclude:
Although associations between Lyme disease and Alzheimer disease, ALS, MS, and Parkinson disease have been proposed by writers of speculative websites and articles, supportive evidence for such an association is lacking. The absence of a positive correlation in the geographic distributions of these conditions provides further evidence against an association between Lyme disease and deaths from these 4 neurodegenerative conditions.
A 2014 study in the Journal of Alzheimer’s also found no positive correlation between Lyme disease and Alzheimer’s disease.
There is also no indication from studies of brain tissue of Alzheimer’s that Lyme-causing bacteria (Borrelia spirochetes) was present. In 2000, NIH researchers found no evidence of Borrelia DNA in samples from 15 patients. In 2017, scientists in Spain examined samples from 10 patients and found no evidence of Borrelia spirochetes via PCR or immunohistochemistry. In 1989, scientists found no evidence of Lyme disease bacteria in samples from six autopsy cases of Alzheimer’s, one case of Pick’s disease, one case of Creutzfeldt-Jakob disease, and four neurologically normal patients.
See also: Review by experts: Lack of Convincing Evidence that Borrelia burgdorferi Infection Causes Either Alzheimer’s Disease or Lewy Body Dementia
Multiple Sclerosis
The MS Society discussed two studies of antibodies in blood that did not indicate that Lyme disease is related to MS. (first study, second study)
MS is a degenerative disease. Delaying appropriate treatment can worsen a patient’s condition. Dr. David Patrick said “we hear of lost vision due to delayed diagnosis of multiple sclerosis because of a false-positive Lyme diagnosis.”
Dr. Steven Novella, Assistant Professor of Neurology at Yale School of Medicine and Executive Editor of Science-Based Medicine, deconstructs claims of Lyme disease causing MS. A Wired reporter recounted what happened when one of Dr. Novella’s patients could not accept a bleak diagnosis of ALS:
After the initial diagnosis, the man left the office, unable to cope with the fact that he had an incurable degenerative disease, likely to kill him within five years. He chose to visit a naturopath instead, who had redemptive news: conventional, narrow-minded medicine had misdiagnosed him. It wasn’t ALS, the naturopath said, but rather chronic Lyme disease, which could be treated with holistic, all-natural supplements.
Nearly a year later, badly degenerated, the man was back in Novella’s office. He’d wasted countless hours and thousands of dollars on false hope. Now, he was willing to listen, but with far less time to prepare for the reality of what lay ahead, and a spirit broken by disappointment.
Autism: No link to Lyme disease
In 2013, scientists analyzed serum samples of 120 children, including 70 with autism and 50 without autism. None of the 120 children tested positive for anti-bodies to Lyme using well established two-tier testing.
The scientists concluded:
The study’s sample size is large enough to effectively rule out the suggested high rates of Lyme disease or associated seroprevalence among affected children.
NIH scientists performed a similar study by looking at 183 children: 104 with autism, 24 with developmental delays, and 55 neurotypical controls. All 183 children tested negative for Lyme antibodies and had no history of Lyme disease.
The NIH scientists concluded:
There was no evidence of an association between Lyme disease and autism.
Thankfully, the “Lyme-Induced Autism Foundation” is now defunct. Sadly, many of the doctors who spoke at “Lyme-Induced Autism” conferences are still practicing.
Resources
General
- CDC: No Geographic Correlation between Lyme Disease and Death Due to 4 Neurodegenerative Disorders, United States, 2001–2010
- Wired: An Alternative-Medicine Believer’s Journey Back to Science
- Obel N, et al. Long term survival, health, social functioning, and education in patients with European Lyme neuroborreliosis: nationwide population based cohort study. BMJ. 2018;361:k1998. (blog, editorial)
- Haahr R, et al. Risk of neurological disorders in patients with European Lyme neuroborreliosis. A nationwide population-based cohort study. Clin Infect Dis. 2019.
- Hellmuth J, et al. The Rise of Pseudomedicine for Dementia and Brain Health. JAMA. 2019
- Infectious Diseases Society of America, American Academy of Neurology, American College of Rheumatology: 2020 Guidelines for the Prevention, Diagnosis and Treatment of Lyme Disease
- Melia MT, et al. Lyme disease: authentic imitator or wishful imitation? JAMA Neurol. 2014.
ALS
- CBC: Former Lunenburg councillor misdiagnosed with Lyme disease now told he has ALS
- Dr. Jeffrey Rothstein: Five myths about ALS
- American Lyme Disease Foundation: Is there a causal relationship between Lyme disease and amylotropic lateral sclerosis (ALS)?
- ALS Untangled: Debunking “When ALS Is Lyme” (podcast)
- ALS Untangled: ALSUntangled update 1: investigating a bug (Lyme Disease) and a drug (Iplex) on behalf of people with ALS.
- Qureshi M, et al. Lyme disease serology in amyotrophic lateral sclerosis. Muscle Nerve. 2009. [paper mirror]
- Visser AE, et al. No association between Borrelia burgdorferi antibodies and amyotrophic lateral sclerosis in a case-control study. Eur J Neurol. 2017.
- Sher HC. The Grace of Denial. NEJM. 2019. (mirror, LymeScience excerpt)
- Maksymowicz S, Siwek T. Diagnostic odyssey in amyotrophic lateral sclerosis: diagnostic criteria and reality. Neurol Sci. 2024.
- Turner MR, Talbot K. Mimics and chameleons in motor neurone disease. Practical Neurology. 2013.
- LymeScience: Tweets on ALS
- TV2: Camilla’s husband was promised a miracle at a German clinic: now he is dead [BCA Clinic and NordicClinic]
- Story of an ALS patient: A warning regarding Body Science Miami [Amy Jaramillo/BodyScience]
- The LymeScience Rogues Gallery features charlatans who have played a role in the targeting of ALS patients:
- Charlene DeMarco, DO
- Gregory P. Bach, DO
- William Lee Cowden, MD [screenshot]
- Dr. Geoffrey Kemp
- Domenick Braccia, DO and Patricia Kane
Alzheimer’s disease
- O’Day DH, Catalano A. A lack of correlation between the incidence of lyme disease and deaths due to Alzheimer’s disease. J Alzheimers Dis. 2014.
- NIH Researchers: Lack of evidence of Borrelia involvement in Alzheimer’s disease.
- Journal of Alzheimer’s Disease: Study Disproves Link Between Lyme Disease and Alzheimer’s
- Haahr R, et al. Dementia in patients with European Lyme neuroborreliosos: Nationwide population-based case control and cohort studies. 2019.
- Pisa D et al. Polymicrobial Infections In Brain Tissue From Alzheimer’s Disease Patients. Sci Rep. 2017.
- Pappolla MA, et al. Concurrent neuroborreliosis and Alzheimer’s disease: analysis of the evidence. Hum Pathol. 1989.
- Gutacker M, et al. Arguments against the involvement of Borrelia burgdorferi sensu lato in Alzheimer’s disease. Res Microbiol. 1998. (mirror)
- McLaughlin R, et al. Alzheimer’s disease may not be a spirochetosis. NeuroReport. 1999.
- Galbussera A, et al. Lack of evidence for Borrelia burgdorferi seropositivity in Alzheimer disease. Alzheimer Dis Assoc Disord. 2008
- Wormser GP, et al. Lack of Convincing Evidence that Borrelia burgdorferi Infection Causes Either Alzheimer’s Disease or Lewy Body Dementia. Clin Infect Dis. 2021.
- Hammond RR, Gage FH, Terry RD. Alzheimer’s disease and spirochetes; a questionable relationship. Neuroreport. 1993 Jul;4(7):840. [questioning Judith Miklossy’s claims]
Multiple Sclerosis
- MS Society statement
- Steven Novella: MS and Lyme disease
- P.K. Coyle, MD (director of MS Comprehensive Care Center at Stony Brook University Medical Center): Lyme Disease and MS: Fact and fiction
- Video: Dr. Brandon Beaber, MD: Multiple sclerosis is not lyme disease
- Willis MS, Bai Y. Confounding issues in the diagnosis of multiple sclerosis: lyme disease testing. Lab Med. 2003;34(6):467-475 [Case of MS initially thought to be Lyme disease]
- Cheema J, et al. Multiple Sclerosis and psychosis: A case report. Mult Scler Relat Disord. 2019.
- Halperin JJ, et al. Lyme neuroborreliosis: central nervous system manifestations. Neurology. 1989
- Coyle PK. Borrelia burgdorferi antibodies in multiple sclerosis patients. Neurology. 1989;39(6):760-761.
- Coyle PK, et al. Significance of reactive Lyme serology in multiple sclerosis. Ann Neurol. 1993.
- MacLean G, et al. Low Seroprevalence of Lyme Disease Among Multiple Sclerosis Patients in New Brunswick. Can J Neurol Sci. 2020.
- Schmutzhard E, et al. Borrelia burgdorferi antibodies in patients with relapsing/remitting form and chronic progressive form of multiple sclerosis. J Neurol Neurosurg Psychiatry. 1988.
- Vatne A, et al. Multiple sclerosis in Vest-Agder County, Norway. Acta Neurol Scand. 2011.
- Lindland ES, et al. Are white matter hyperintensities associated with neuroborreliosis? The answer is twofold. Neuroradiology. 2024.
- Makarov C, et al. Early comorbidities and diagnostic challenges in people with multiple sclerosis with possible impact on disease management. Mult Scler J Exp Transl Clin. 2025.
Autism
- Ajamian M, et al. Serologic markers of Lyme disease in children with autism. JAMA. 2013
- Ajamian M, et al. Autism and Lyme disease–reply. JAMA. 2013.
- The Scientist: Autism-Lyme Correlation Debunked
- NIH scientists: Lack of Serum Antibodies against Borrelia burgdorferi in Children with Autism
- American Lyme Disease Foundation: Does Lyme disease induce autism in children?
- Thinking Person’s Guide to Autism: Pseudoscience Alert: Lyme-Induced Autism
- Dr. Mark Hoofnagle: Medical Hypotheses—“just make shit up; we’ll publish it” [Debunks Bransfield’s paper trying to connect Lyme and autism]
- Autism Science Foundation: Beware of Non-Evidence-Based Treatments
- General info about Lyme disease in Children: AAP Review
Parkinson’s disease
- Dr. Bill Stamey, MD: Lyme and parkinsonism: is there a connection?
Updated May 19, 2025