Table of contents
CD57 tests are not a good idea.
Why? Because at least two studies show CD57 can’t tell the difference between people who would be considered to have chronic Lyme disease and others. Whether CD57 is considered low or high, it’s irrelevant to Lyme disease.
Therefore, relying on a CD57 test could result in false positives or false negatives. That’s why the CDC, North American medical experts, European science organizations, and the Royal College of Pathologists of Australasia explicitly warn against CD57 and other unvalidated tests.
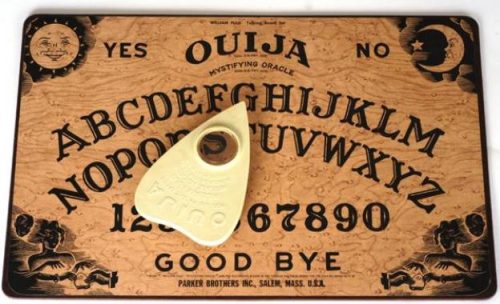
CD57: Like a Ouija board
In the 1960s and 1970s, Ouija boards became popular as a seemingly supernatural way to receive answers to questions. However, scientific, unbiased testing using a blindfold revealed the truth: Ouija is entertaining but not paranormal at all.
The apparent efficacy of the Ouija board was due to psychology and the ideomotor phenomenon, unconscious motions that are thought (falsely) to be caused by paranormal activity.
We humans want to find explanations to every mystery, especially when the mystery revolves around our health. It’s frustrating having unexplained symptoms and not knowing what to do about them. Because of false information online, people sometimes are led to believe any possible symptom means Lyme disease.
The CD57 test is advertised as a way to confirm—in a sciency-sounding way—a Lyme diagnosis. But the CD57 test is as useless as a Ouija board for determining if someone is infected with Borrelia Burgdorferi, the bacteria that cause Lyme disease.
A positive diagnosis provides relief, feelings of empowerment, and an apparent way forward. But a chronic Lyme diagnosis is ultimately a mirage.
The Evidence
A Canadian Study
In 2015, scientists in British Columbia, Canada compared 4 groups of patients: 13 patients with the “Alternatively diagnosed chronic Lyme syndrome” (ADCLS), 25 patients with Chronic Fatigue Syndrome (CFS), 25 matched healthy control patients, and 11 Lupus control patients. The researchers found none of the ADCLS patients had signs of Lyme disease and noted that they “have a similar phenotype to that of CFS patients.” They also discussed CD57 tests:
Some practitioners employ CD57 cell count as an additional criterion to support diagnosis of ADCLS. Our finding of no significant difference in CD57 cell counts between ADCLS and CFS patients and healthy controls is consistent with another study that could not replicate the findings on which such practice is based.
A US Study
The Canadian study above referenced a 2009 study by NIH scientists entitled “Natural Killer Cell Counts Are Not Different between Patients with Post-Lyme Disease Syndrome and Controls.” The scientists compared three groups of patients: 9 patients with post-Lyme disease syndrome (PLDS), 12 patients who recovered from Lyme disease, and 9 healthy volunteers. The results were definitive:
We conclude that the numbers of NK cells do not differ between patients with PLDS, individuals who have recovered from Lyme disease, and healthy volunteers and that the number of CD57+ non-T (CD3−) cells is not helpful in evaluation or management of these patients.
Two French Reviews
Another 2018 French review looked at 16 different diagnostic guidelines from 7 countries. None of the guidelines recommended CD57 testing.
In 2019, French scientists reviewed the scientific literature published between 1983 and 2018 about “unconventional” Lyme Borreliosis (LB) testing, including CD57. The scientists concluded:
CD57-marker specificity [ability to rule out false positive results] for LB is probably low, because low CD57 levels were also found in patients with numerous autoimmune diseases, infections or cancers.
CD57 measurement does not seem useful, even after antibiotics or for persistent symptoms. To our knowledge, no study has provided this test’s performance (sensitivity/specificity).
“Chronic Lyme” organization doesn’t recommend CD57 testing
Even the pseudoscience group German Borreliosis Society (Deutsche Borreliose-Gesellschaft, DBG) did not recommend CD57 testing. The DBG states:
It is not possible to evaluate the CD57+ NK cells as a laboratory parameter in connection with Lyme borreliosis at present, on account of the insufficient data available.
Conclusion: CD57 testing for Lyme is discredited
Online groups, many with the word “Lyme” in their names, have deceptively promoted CD57 testing as valid for Lyme disease while spreading false and misleading information about well-established testing.
Established testing is useful, but it must be used correctly. According to the CDC:
- Patients who have had Lyme disease for longer than 4-6 weeks, especially those with later stages of illness involving the brain or the joints, will almost always test positive.
- A patient who has been ill for months or years and has a negative test almost certainly does not have Lyme disease as the cause of their symptoms.
- Serologic testing is generally not useful or recommended for patients with single EM rashes. For this manifestation, a clinical diagnosis (alone) is recommended.
See also the following LymeScience pages:
- Lyme disease tests: Science vs Misconceptions
- How chronic Lyme recruits followers
- Lyme misdiagnosis illustrated
- Red flags of chronic Lyme quackery
- CDC scientist: Why bands 31 and 34 aren’t used to test for Lyme disease
References
CDC: Laboratory tests that are not recommended
Moore A, et al. Current Guidelines, Common Clinical Pitfalls, and Future Directions for Laboratory Diagnosis of Lyme Disease, United States. Emerging Infect Dis. 2016.
Marques A, et al. Natural killer cell counts are not different between patients with post-Lyme disease syndrome and controls. Clin Vaccine Immunol 2009;16:1249–1250.
Patrick DM, et al. Lyme Disease Diagnosed by Alternative Methods: A Phenotype Similar to That of Chronic Fatigue Syndrome. Clin Infect Dis. 2015;61(7):1084-91.
University of Vermont Medical Center: Sample Collection for CD57 for Lyme Disease no longer Available via UVM Medical Center
NIH scientists respond to a bizarre and flawed letter from Raphael Stricker, former ILADS president.
Nielsen CM, et al. Functional Significance of CD57 Expression on Human NK Cells and Relevance to Disease. Front Immunol. 2013;4:422.
Eldin C, et al. Review of European and American guidelines for the diagnosis of Lyme borreliosis. Med Mal Infect. 2018.
Raffetin A, et al. Unconventional diagnostic tests for Lyme borreliosis: a systematic review. Clin Microbiol Infect. 2019;
LTT y CD3-/CD57+ en el diagnóstico de la enfermedad de Lyme. (LTT and CD3-/CD57+ in the diagnosis of Lyme disease.)