Short answer: No
Key points—Rocky Mountain spotted fever is:
- a deadly tick-borne infection that requires prompt treatment.
- treated with a short course of antibiotics and not “chronic” or “persistent”.
- not a Lyme co-infection because it is spread by different ticks.
- an illness that usually results in symptoms 3-12 days after the bite of an infected tick.
Please refer to the CDC for detailed information on symptoms.
This is an article originally published in April 2018 by Dr. Phillip Baker, PhD, the Executive Director of the American Lyme Disease Foundation (ALDF).
The full PDF of this article may be downloaded from the ALDF.
During the past few months, we have received several inquiries from individuals who: (a) claim to have nonspecific symptoms of many months to years in duration; (b) are seronegative for Lyme disease; and, (c) are seropositive for Rocky Mountain Spotted Fever (RMSF) based on the results of approved diagnostic laboratory tests. Since their symptoms are not resolved by treatment with a short course of recommended antibiotics, they believe that extended antibiotic therapy is required to cure what they believe to be “chronic RMSF”.
It should be noted that RMSF is a serious, life threatening infection that often is fatal if not diagnosed and treated promptly (1). There is no possibility that acute RMSF is ever likely to advance to a chronic stage of illness. In a recent report (2), investigators at the Centers for Disease Control and Prevention (CDC) provide a satisfactory and reasonable explanation for what may be happening in such individuals.
In 1973, investigators isolated a rickettsial organism, designated as WB-8-2 T , from adult Amblyoma americanum (lone star) ticks in a recreational area in Tennessee (3, 4). Subsequently, WB-8-2 T was identified in 16% of A. americanum ticks in South Carolina, and in 11% and 41% of A. americanum ticks in Tennessee and Arkansas, respectively. Note that although lone star ticks transmit RMSF as well as other rickettsial infections, they do not transmit Lyme disease (5). Since the results of several taxonomic and molecular studies revealed a number of isolates very similar to WB-8-2 T , it was given the name of Rickettsia amblyommatis sp. nov to designate it as a distinct taxonomic entity that shares antigens with the spotted fever group of rickettsiae (6). It occurs in several tick species of the genus Amblyoma throughout the Western hemisphere, but is most commonly detected in A. americanum with rates of infection that often exceed 40% of questing adult ticks (2).
Amblyoma americanum is a common human-biting tick. The high prevalence of R. amblyommatis in this tick may complicate the diagnosis and surveillance of other spotted fever type rickettisial infections in humans. Most cases of RMSF are diagnosed using serological assays, and it has been suggested that the cross-reactivity of antibodies to strains like WB-8-2 T against R. rickettsia antigen may help explain the large number of “mild RMSF” cases in areas where A. americanum is prevalent (7-11).
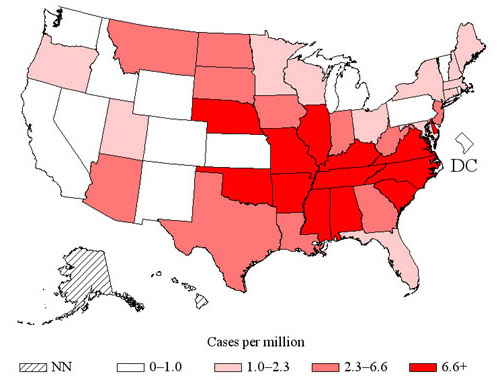
The recommended treatment for RMSF consists of the administration of 100mg oral doxycycline (twice per day) for 5-7 days as the minimum, followed by continued treatment for at least 3 days after the fever has subsided and there is evidence of clinical improvement (12). Since infections caused by R. amblyommatis are usually mild and often do not require treatment, there are no compelling reasons to exceed the regimen used for the treatment of RMSF. Perhaps it would be prudent for those who believe that their symptoms are due to “chronic RMSF”, to consult with their primary care physician to consider the possibility of past exposure to R. amblyommatis and other causes for their symptoms. Note that the lone star tick is widely distributed in the U.S., including areas where Lyme disease is endemic (13).
1. CDC: Rocky Mountain Spotted Fever
2. Karpathy, S, Slater, KS, Goldsmith, SG, Nicholson, WL, and Paddock, CD. Rickettsia amblyommatis sp. nov. : a spotted fever group of Rickettsia associated with multiple species of Amblyomma ticks in North, Central, and South America. Int. J. Syst. Evol. Microbiol. 2016: 66; 5236-5243.
3. Burgdorfer, W, Cooney, JC, and Thomas, LA. Zoonotic potential (Rocky Mountain spotted fever and tularemia) in the Tennessee Valley region. Am. J. Trop. Med. Hyg. 1974: 23; 109-117.
4. Burgdorferi, W, Hayes, SF, and Thomas, LA. A new spotted fever group rickettsia from the lone star tick, Amblyomma americanum. In: Burgdorfer, W, Anacker, RL, editors. Rickettsiae and Rickettsial Diseases. New Yor: Academic Pres, Inc. 1981. Pp 595-602.
5. CDC: Lyme transmission
6. Oren, A, Vandamme, P, and Schink, B. Notes on the use of Greek word roots in the genus and species names of prokaryotes. Int. J. Syst. Evol. Microbiol. 2016: 66; 2129-2140.
7. Apperson, CS, Engber, B, Nicholson, WL, Mead, DG, Engel, J, Yabsley, MJ, Dail, K, Johnson, J, and Watson, DW. Tick-borne diseases in North Carolina: is Rickettsia amblyommii a possible cause of rickettsiosis reported as Rocky Mountain spotted fever? Vecto Borne Zoonotic Dis. 2008: 8; 597- 606.
8. Delisle, j, Mendell, NL, Stull-Lane, A, Bloch, KC, Bouyer, DH, and Moncayo, AC. Human infections by multiple spotted fever group Rickettsiae in Tennessee. Am. J. Trop. Mede. Hyg. 2016: 94; 1212-1217.
9. Openshaw, JJ, Swerdlow, DL, Krebs, JW, Holman, RC, Mandel, E, Harvey, A, Haberling, D, Massung, RF, and McQuiston, JH. Rocky Mountain spotted fever in the United States, 2000- 2007; interpreting contemporary increases in incidence. Am. J. Trop. Med. Hyg. 2010: 83; 174- 182.
10. Parola, P, Paddock, CD, Socolovschi, C, Labruna, MB, Mediannikov, O, Kernif, T, Abdad, MY, Stenos, J, and Bitam, I et al. Update on tick-borne rickettsiosis around the world: a geographic approach. Clin. Microbiol. Rev. 2013: 26; 657-702.
11. Stromdahl, EY, Vince, MA, Billingsley, PM, Dobbs, NA, and Williamson, PC. Rickettsia amblyommii infecting Amblyomma americanum larvae. Vector Borne Zoonotic Dis. 2008: 8; 15- 24.
12. CDC: Tick-borne Diseases of the United States, 2017
13. CDC: Geographic distribution of ticks that bite humans
Other relevant resources
Dahlgren FS, et al. Fatal Rocky Mountain spotted fever in the United States, 1999-2007. Am J Trop Med Hyg. 2012;86(4):713-9.