Below is a chart mapping tick-borne infections in the USA to the ticks known to spread the infections to humans. Many of these infections and ticks are highly geographically restricted.
Victims of chronic Lyme quackery frequently are led to believe falsely that they have multiple co-infections, even ones that are not known to be transmitted together.
For example, reality TV star Yolanda Hadid was diagnosed with about 2 dozen different infections. The New York woman in this short video clip was convinced that she had received an impossible combination of chronic Lyme disease and 6 co-infections from a single tick:
The chart below is useful to explain why the beliefs of those diagnosed with chronic Lyme and co-infections are not supported by scientific evidence. According to the CDC Lyme FAQ:
“There is, however, a great deal of misinformation regarding tickborne coinfections on the internet. The possibility of having three or more tickborne infections or having pathogens such [as] Bartonella or Mycoplasma (which have not been shown to be tickborne), is extremely unlikely.”
Survey results defy reality
In 2013, a pseudoscience propaganda group called LymeDisease.org surveyed people claiming to have chronic Lyme disease (CLD), a condition not recognized by medical science. LymeDisease.org narrowed its sample to 3090 individuals who met a set of criteria and published the data in PeerJ.
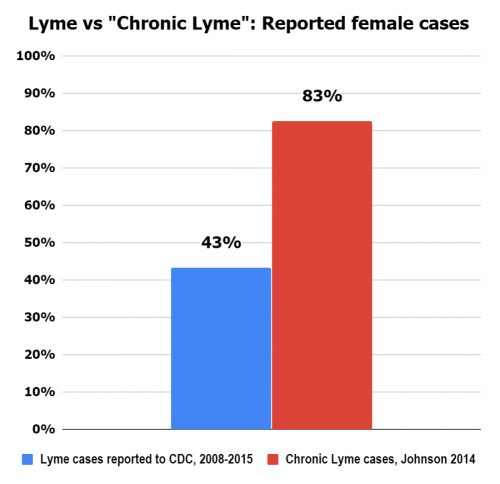
The results were shocking in how implausible they are. Of the 3090 individuals claiming to have CLD:
- 83% were female, compared to 43% of CDC reported Lyme cases being female.
- 54% claimed to have Bartonella coinfections, despite Bartonella not being a known tick-borne disease or Lyme co-infection. And most cases of real Bartonella (typically spread by cats) go away on their own, though short-term treatment may be warranted.
- 19% claimed to have Mycoplasma coinfections despite Mycoplasma not being a known tick-borne disease or Lyme co-infection.
- 20% claimed to have Ehrlichia coinfections despite Ehrlichia not being transmitted by Lyme-carrying Ixodes ticks, except for possibly the rare Ehrlichia muris eauclairensis bacteria detected only in Wisconsin and Minnesota with 39 reported cases from 2009-2014.
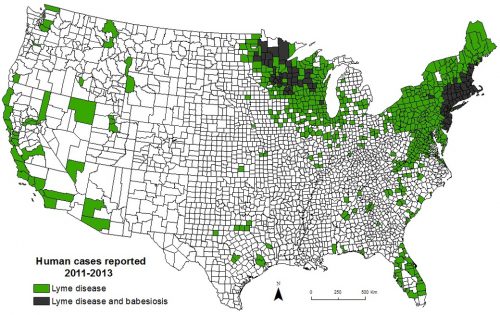
- 56% claimed to have Babesia coinfections despite the different geography of confirmed Babesia cases from the surveyed population.
- 7% claimed to have Rocky Mountain Spotted Fever, despite this disease not being a known Lyme co-infection.
- 1% claimed to have Tularemia, despite this disease not being a known Lyme co-infection
Of course, all of the above infections are curable with a few weeks of anti-microbial treatments, at most, even if the individuals really did have these improbable combinations of co-infections.
Chronic Lyme advocates like to use real flaws in antibody testing for Lyme disease to pretend that the testing is worthless. However, the CDC emphasizes, “It is not until 4 to 6 weeks have passed that the test is likely to be positive. This does not mean that the test is bad, only that it needs to be used correctly.”
Victims of chronic Lyme quackery typically claim to have had Lyme disease for months or years. In the event of a real late Lyme infection, antibodies would invariably be detectable. Unfortunately, many victims of chronic Lyme quackery are told to ignore or misinterpret their negative tests, which are likely true negatives.
However, the misleading talking point made by chronic Lyme advocates about antibody testing is irrelevant for one of their favorite fictional co-infections, chronic Babesia, which would be directly visible in a microscope if it was there.
(This chart is horizontally scrollable)
|
Causative agent (condition) |
Chronic infection after science-based anti-microbial treatment? | Black-legged tick (Ixodes Scapularis) | Western black-legged tick (Ixodes Pacificus) | American dog tick (Dermacentor variabilis) | Rocky Mountain wood tick (Dermacentor andersoni) | Brown dog tick (Rhipicephalus sanguineus) | Lone star tick (Amblyomma americanum) | Groundhog tick (Ixodes cookei aka woodchuck tick) | Gulf coast tick (Amblyomma maculatum) | Soft tick (Ornithodoros spp.) |
| Borrelia burgdorferi (Lyme disease) | no | ❌ | ❌ | |||||||
| Babesia microti (Babesiosis) | no | ❌ | ||||||||
| Ehrlichia ewingii (Ehrlichiosis) | no | ❌ | ||||||||
| Ehrlichia chaffeensis (human monocytic ehrlichiosis) | no | ❌ | ||||||||
| Anaplasma phagocytophilum (Anaplasmosis) | no | ❌ | ❌ | |||||||
| Francisella tularensis (Tularemia*) | no | ❌ | ❌ | ❌ | ||||||
| Rickettsia rickettsii (Rocky mountain spotted fever) | no | ❌ | ❌ | ❌ | ||||||
| Rickettsia parkeri (spotted fever) | no | ❌ | ||||||||
| Borrelia Hermsii (Tick-borne relapsing fever) | no | ❌ | ||||||||
| (STARI) | no *** | ❌ | ||||||||
| Borrelia miyamotoi | no | ❌ | ❌ | |||||||
| Borrelia mayonii (Lyme disease) | no | ❌ | ||||||||
| Ehrlichia muris eauclairensis | no | ❌ | ||||||||
| Heartland virus | n/a ** | ❌ | ||||||||
| Powassan virus and Deer Tick Virus | n/a ** | ❌ | ❌ | ❌ | ||||||
| Colorado Tick Fever virus | n/a ** | ❌ | ||||||||
| Alpha gal (meat allergy) | n/a ** | ❌ |
* Tularemia can also be transmitted by biting flies and infected animals
** Viruses and meat allergies cannot be treated with antimicrobials. Meat allergy may persist for some time.
*** It is unclear if antibiotics are warranted at all for STARI. And no pathogen has been detected as the cause of STARI.
Some rare infections such as Bourbon Virus are not listed above. Information about other infections can be found at the CDC. Also not listed is the emerging east Asian longhorned tick (Haemaphysalis longicornis), which has spread on the east coast United States.
Conditions frequently falsely diagnosed as “co-infections” or “associated diseases” of Lyme disease.
| Bartonella | Not a tick-borne disease |
| Mycoplasma | Not a tick-borne disease |
| Mold or sick building syndrome | No relation to tick-borne diseases and usually a scam |
| Biotoxin illness or Chronic Inflammatory Response Syndrome (CIRS) | An unrecognized diagnosis made up by Ritchie Shoemaker, a doctor who stopped practicing medicine after disciplinary action from the Maryland Medical Board |
| Other unsubstantiated toxins | Generally scams based on a misunderstanding of biology |
| Heavy metals | No relation to tick-borne diseases and usually a scam |
| Morgellons | Not a real diagnosis |
| Electomagnetic hypersensitivity (e.g. WiFi or cell phone allergies) | Not a real diagnosis |
| Kryptopyrroluria aka Hemopyrrollactamuria aka pyroluria aka Pyrrole disorder aka mauve factor | Not a real diagnosis |
| Protomyxzoa Rheumatica | Not a real diagnosis |
| Multiple Chemical Sensitivity | Not a real diagnosis |
| Adrenal fatigue | Not a real diagnosis |
| Candida overgrowth | Generally a fake condition diagnosed by quacks |
| Leaky gut | A hypothesized condition usually diagnosed by quacks without compelling evidence |
| MTHFR | A gene mutation that has been falsely blamed on everything. While treatment is rarely needed, it is easily treated with inexpensive B vitamin supplements. |
| MARCoNS | Not a real diagnosis |
Please see further explanations at our Co-infection Confusion page.
Also, many real diseases have been falsely blamed on Lyme disease. Despite claims by chronic Lyme believers, there is no link between Lyme disease and any of a myriad of conditions including: autism, ALS, MS, Alzheimer’s, and Parkinson’s.
Resources:
CDC: Geographic distribution of ticks that bite humans
CDC: Infection surveillance maps
CDC: Tick-borne Diseases of the United States (reference manual)
CDC: Tickborne Diseases of the United States
Dr. Lantos and Wormser: Chronic Coinfections in Patients Diagnosed with Chronic Lyme Disease: A Systematic Review
Biggs HM, et al. Diagnosis and Management of Tickborne Rickettsial Diseases: Rocky Mountain Spotted Fever and Other Spotted Fever Group Rickettsioses, Ehrlichioses, and Anaplasmosis – United States. MMWR Recomm Rep. 2016;65(2):1-44.
Updated May 23, 2024